EoE is a chronic, long-term health condition that can be lifelong. There is no known cure, however, there are treatment options available that can help control the symptoms of EoE, inflammation of the esophagus and protect it from future complications.
EoE can be treated by medications, dietary management, or a combination of these to help control the inflammation, decrease symptoms and decrease the risk of food impactions and narrowing of the esophagus (strictures).
Medication
Medications may include:
Proton-pump inhibitors (PPIs)
PPIs are oral medications, sometimes called acid blockers, which are often tried as a first-line treatment for children and adults with EoE.
It is important to know that while not perfectly understood, PPIs seem to have ways of working on the esophagus that help patients with EoE beyond decreasing acid production.
Swallowed topical steroids
Several different topical or swallowed corticosteroids (budesonide or fluticasone) are very effective medications and help control inflammation in the majority of EoE in most patients. These medications are taken by either an asthma type pump (meter dose inhaler) and are swallowed rather than inhaled, or mixed into a thicker solution/slurry which is swallowed, to coat the esophagus.
Budenoside is the only approved corticosteroid for the treatment of EoE in adults and is available in tablet form. It is a rapidly-dissolving tablet, taken twice daily after meals which dissolves in the mouth and coats the esophagus to help reduce inflammation. Regardless of the form of topical steroid, the patients should not eat or drink for at least 30 minutes after taking the medication and it can be used long-term to treat EoE.
Biologic medication
In severe cases, a biologic medication called dupilumab can be given through an intramuscular injection to block the allergic response causing EoE.
Dietary management
Because in some cases EoE can be triggered by an allergic response to certain foods, eliminating only these foods that cause inflammation in the esophagus can help to control inflammation and reduce symptoms. As a result, the symptoms and inflammation may go away without the need for medications if people stick to the diet. However, it can be difficult to pinpoint the exact foods that act as a trigger. And even if the trigger foods are determined, it can often be very challenging for most people to maintain the diet over the long-term.
Another challenge is that a person with EoE may have one or more foods or allergens triggering their EoE. They can help potentially identify the trigger foods that may be causing EoE by eliminating them one by one or in groups and undergoing repeat endoscopy and biopsies. The elimination diet after the initial scope and subsequent scopes are to try to identify the trigger foods. (See section on Elimination diet).
It is important to know that traditional allergy tests (skin and blood) are not useful to identify EoE related to food triggers, because in the context of EoE they can give false positive results and generate confusion. Such tests are used to help diagnose IgE mediated food allergy (those at risk of anaphylaxis), not a non-IgE mediated food allergy like EoE. As such, these allergy tests are not recommended to guide food elimination treatment for patients with EoE.
Dietary management may include:
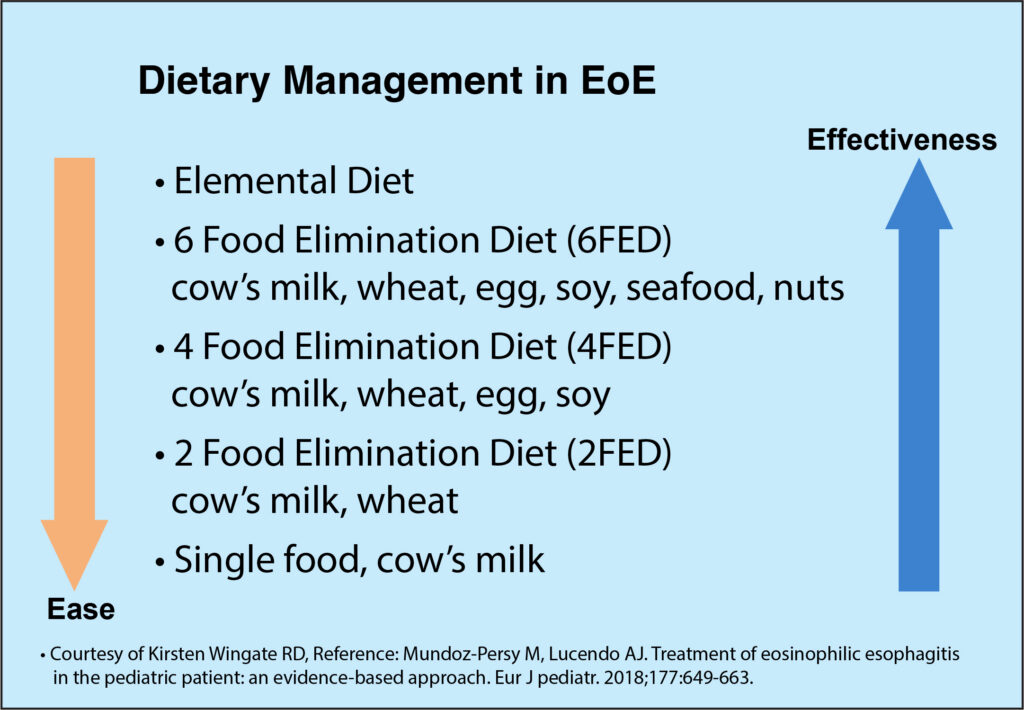
Elimination diet
With this approach, common food allergens are excluded from the diet for a period of time (usually a few months) after being diagnosed, then the person is re-evaluated by endoscopy to see if there is a significant reduction in eosinophils. If successful, select foods are added back in one (or two) at a time, with repeat endoscopy at each stage to determine the trigger(s). Then, identified trigger(s) would be avoided over the long-term to help control inflammation and manage symptoms.
Sometimes a 1 or 2 food elimination diet is the first step, as this involves a smaller change in the diet while targeting the most likely triggers (milk and/or wheat). While there is a greater response rate by starting out with a 4 or 6 food elimination, this should be balanced with the increased difficulty of more dietary restrictions.
In addition, the likelihood of EoE improvement from avoiding nuts (peanut / tree nuts) and seafood (fish / shellfish) is not as great as it would be from avoiding other allergens like cow’s milk. Therefore, the degree of additional benefit from avoiding nuts and seafood needs to be carefully balanced with the potential additional risk of future development of IgE mediated food allergy and the risk of anaphylaxis to these foods during a period of prolonged avoidance, especially in patients with a history of allergic conditions.
This balance of benefits and risks should be especially discussed with atopic patients (those with a predisposition toward developing allergic conditions), before elimination diets are considered. For example, unnecessarily removing peanut from the diet of a young atopic child in the hopes of improving EoE can have the undesired effect of increasing the risk of developing an IgE-mediated allergy with the potential for anaphylaxis. The only way to prevent future peanut allergy currently is to introduce it early and eat it regularly (e.g. several times a week).
- The elimination diet approach helps determine which food(s) are contributing towards inflammation in the esophagus and generally helps control symptoms in children and adults.
An elimination diet requires discipline and motivation, and can be difficult to maintain. Working together with a dietitian is key and will ensure proper substitutions and adequate nutrition. A dietitian can help guide individuals and parents who decide to make diet changes. For example, by eliminating milk and dairy only (an important source of nutrients like protein, fat, vitamin D, calcium, B12), you will need to compensate and find substitutes like fortified plant-based beverages such as oat or soy milk. In some cases, a specialty formula may need to be considered, as fortified milk substitutes are not recommended for children younger than 2 years of age.
Talk to your healthcare team and dietitian about the best plan for you or your child.
If you need to avoid certain foods, read ingredient lists carefully when grocery shopping, and make sure to communicate what you are avoiding when ordering from restaurants.
- Check out our article with Kirsten Wingate, RD on dietary management of EoE:
- Ask the dietitian: Dietary management for those with Eosinophilic Esophagitis (EoE)
- Read our article with Linda Kirste, RD on optimizing nutrition in kids with EoE or Food Protein-Induced Enterocolitis Syndrome (FPIES):
- Tips for optimizing nutrition in children living with FPIES or EoE
Here are a few meal ideas for people who are avoiding milk, egg, soy and wheat:
Double check labels of any store-bought foods to make sure there are no ingredients which you need to avoid.
Note: There is a risk that someone who has wheat as a trigger for their EoE might also react to gluten that is found in rye and barley. If you need to eliminate wheat from your diet, talk to your doctor to understand whether you need to also eliminate gluten from your diet.
Breakfast

- Wheat/Gluten-free bread* (check ingredients) + dairy-free margarine/jam/honey
- Wheat/Gluten-free oatmeal* or hot oat bran
- Try adding: oat milk, maple syrup, berries
- Fresh fruit or orange juice
- Hash browns
- Wheat/Gluten-free breakfast cereal* (check ingredients) or granola + oat milk/amino acid-based infant formula/dairy-free, pea-based milk
- Breakfast sausage (check ingredients)
- ‘Breakfast hash’ – meat, potatoes, vegetables fried in a skillet
- Smoothies (recipes below)
Lunch

- Any meats without added ingredients
- Sandwich made with wheat/gluten-free bread* – try hummus, lunch meats (check ingredients) and vegetables as toppings
- Potato salad/bean salad with homemade sauces
- Wheat/Gluten-free pasta salad* with homemade vinaigrette
- Home-made soup or chili (check ingredients of broth/seasoning cubes)
- Homemade congee (rice porridge)
- Rice paper rolls
- Dinner leftovers
Snacks

- Corn tortilla chips + salsa/guacamole
- Veggie sticks + hummus/white bean dip
- Fresh fruit
- Apple sauce
- Wheat/Gluten-free crackers* with seed butter (tahini, sunflower, etc.)
- Dried fruit
- Potato chips
Dinner

- Rice/quinoa with meat and vegetables
- Wheat/Gluten-free pasta* with olive oil and garlic or meat sauce or meat balls and tomato sauce
- Spaghetti squash (instead of spaghetti) and tomato sauce
- Potatoes / sweet potatoes / turnips
- Chili (beans and meat)
- Tacos made with soft corn tortillas (bean, meat, or veggie fillings) – top with avocado, salsa, cilantro, lime etc.
- Cooked veggies, fresh salads
- Chick pea/bean dishes
- Meat dishes
- Pork with onions and apples
- Chicken stew (Moroccan, French, etc.)
- Grilled steak
- Cabbage rolls
- Wheat/Gluten-free Sheppard’s Pie*
*Remember to check with your doctor about whether you need to avoid wheat, gluten or both.
Modified Texture Tips
If you are struggling with swallowing, consider the following ideas to see if you can increase your intake:

- Try thick smooth foods like:
- Breakfast: oatmeal, smoothies
- Lunch: blended soups
- Dinner: mashed potatoes, blended soups
- Snacks: Meal replacement beverages, smoothies, apple sauce
- If the foods above are okay, you can add soft, moist foods, and cut them very small:
- Breakfast: hash browns, sausage meat (take out of casing and fry like ground sausage meat)
- Lunch: chili, potato salad, pasta salad
- Dinner: soft-cooked pasta with sauce, rice, ground beef/chicken, soft-cooked vegetables cut up small
High Calorie Smoothie Recipes:
Berry Blend

- 1 frozen banana
- ½ cup frozen berries
- 1 cup of oat milk or alternative milk
- Protein boost: 2 Tbsp hemp hearts or 2 Tbsp tahini (contains sesame)
- Calorie boost: 3 Tbsp coconut ice cream/coconut yogurt/coconut milk (from can), or 2 Tbsp coconut oil, or ¼ cup frozen avocadoes
Tropical Blend

- 1 frozen banana
- 1 can of canned pineapple or peach, or ½ cup frozen tropical fruit
- 1 cup or more of liquid (mango juice or milk alternative)
- Protein boost: 2 Tbsp hemp hearts or 2 Tbsp tahini (contains sesame)
- Calorie boost: 3 Tbsp coconut ice cream/coconut yogurt/coconut milk (from can), or 2 Tbsp coconut oil, or ¼ cup frozen avocadoes
Recipes provided by Kirsten Wingate RD, B.C. Children’s hospital.
- Visit allergicliving.com/recipes for delicious recipe ideas. The recipes on this site can be filtered by allergen.
- allergicliving.com/recipes
Elemental diet
An elemental diet involves replacing all foods in the diet with a prescribed liquid specialized formula diet. These formulas are made up of broken-down proteins called amino acids. The elemental diet is effective at reducing inflammation but is costly, difficult to maintain, and limits many social aspects of eating. Amino acid formulas can also be used as a supplement during other elimination diet stages to add extra nutrition. In general, an elemental diet is meant to be used short-term only (elemental formulas may be used for a few years as a supplement especially with very young children).
Dilation
Some people with EoE develop a narrowing of the esophagus which causes further issues with swallowing and choking. Dilation is an endoscopic procedure in which a narrowing (or stricture) is stretched to widen the esophagus and to allow food to pass more comfortably. This does not deal with the underlying inflammation, but can help symptoms to improve at least in the short-term.
- Please speak with your doctor to discuss all treatment options and determine the ones that are most suitable for you or your child.